introduce
Eating disorders are identified when children cannot or refuse to consume sufficient amounts or types of solids and liquids to maintain proper nutrition . Complications of feeding problems range from mild (for example, missed meals) to severe (for example, severe malnutrition). About 25-35% of normal development parenting children and up to 80% of patients with developmental disorders of eating difficulties. Feeding disorders may manifest as complete refusal to eat, dependence on supplementary feeding (such as a gastrostomy tube), inappropriate mealtime behavior, and selection of type and texture.
Subject
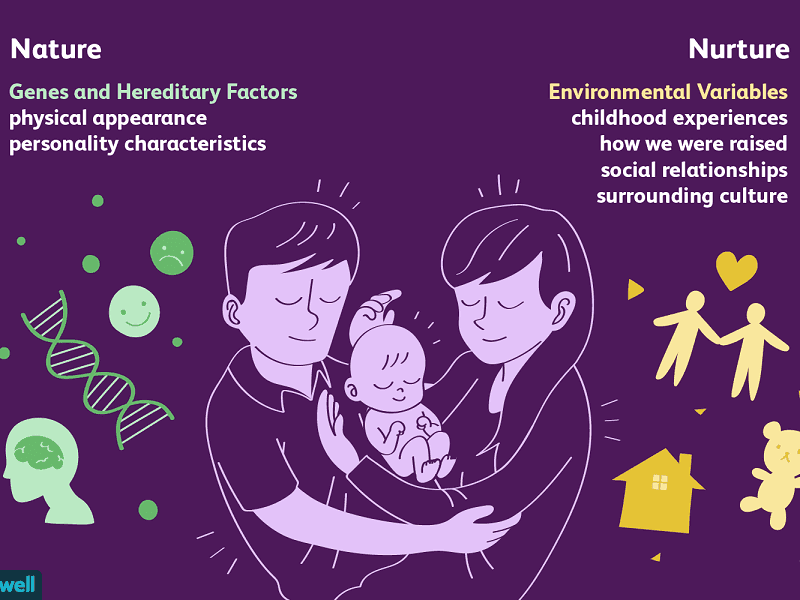
The causes of feeding disorders are also diverse. Feeding problems are usually caused by many interacting biological and environmental factors. For example, Rommel et al. We evaluated 700 children who were referred to the interdisciplinary feeding team and found that more than 60% of the patients had a combined cause of feeding problems (such as medical treatment , behavior, oral exercise).
Biological factors may include early medical procedures, chronic hospitalization, or medical problems that cause eating pains. Even after treating the painful medical condition, the child may continue to refuse food because if the child never or rarely eats, he or she never learns that eating is no longer painful. If a child refuses to eat, he or she will not have the opportunity to practice eating, nor will he or she develop the skills to become a capable eater. Refusal to eat can lead to growth failure, which can lead to poor feeding skills, because malnourished children lack energy for energy consumption. Therefore, in a cycle of development, the child refuses food, does not know that eating is no longer painful, misses the opportunity to develop oral motor skills, and does not gain weight.
problem
Even if the cause of the food refusal is a painful medical condition, the caregiver’s reaction to the child during the meal may make the problem worse. Square and colleagues observed the caregivers and children’s feeding problems during meals, which shows that caregivers use various strategies to encourage eating, such as distraction, coaxing, and condemnation; give children regular rest or avoid eating; and provide preferred food or Toy. All children show refusal behavior and eat food infrequently. When the square waits for people. Analyzed the influence of the behavior of the caregiver in the diet on the feeding behavior of the children, and the results showed that the strategies listed above by the strategists to encourage eating actually worsened the behavior of 67% of children.
Given the relationship between the cause of the feeding problem and the behavior of the caregiver, these results are not surprising. Parental strategies, such as stopping meals or coaxing, may have a direct effect on temporarily preventing bad child behavior. From a child’s point of view, research by Piazza et al. It is recommended that if the refusal produces a “good outcome” for the child (for example, the end of the meal), the refusal will continue.
Research Background
The treatment strategy with the most scientific support is based on behavioral analysis. Kerwin, Volkert and Piazza reviewed the research literature on the treatment of feeding disorders in children to determine which treatments have sufficient scientific support to be labeled “effective”. Kerwin and Volkert and Piazza found that behavioral interventions are the only treatment with sufficient scientific evidence Methods Similar analyses by Sharp and his colleagues, Ledford and Gast, and Williams and colleagues support those of Kerwin, Volkert, and Piazza.
Research results and conclusions
Since children have feeding problems for various reasons, treatment should focus on all the components that cause feeding problems (i.e. biology, oral movement, and psychology) and should be interdisciplinary. A preliminary analysis of the results of 50 children admitted to the interdisciplinary day treatment feeding program showed that more than 87% of the treatment goals were met through discharge from the program. When the increase in calories burned by the oral cavity was the goal of treatment, 70% of patients reached the goal. Even if the child does not reach the 100% oral intake target, their oral intake level is greatly improved and is within 20% of the target. One hundred percent of patients achieved the goal of increasing texture, reducing bottle dependence, increasing self-feeding skills, and increasing food consumption.
All patients receiving nutrition through the tube will be reduced by tube feeding, and 70% of patients have reached the goal of reducing tube feeding. Patients who enter the procedure with a nasogastric tube either leave the procedure without the tube (75%) or have the tube removed soon after discharge (100%). Ninety-seven percent of patients achieved the goal of reducing inappropriate mealtime behaviors. 88% of the nursing staff received training to implement the treatment, the accuracy rate was over 90%, and the treatment was successfully transferred to the family and the community in 100% of the cases.
Follow-up data indicate that most patients continue to make progress in age-typical feeding (for example, increase in size, decrease in gastrostomy tube feeding, and start self-feeding). Williams and colleagues, Greer and colleagues, and Laud and colleagues provided similar data in which interdisciplinary treatment and behavior analysis focused on children with severe feeding problems that produced positive results.
Enlightenment
The interdisciplinary, intensive treatment of pediatric feeding disorders has successfully improved various feeding problems, including dependence on supplementary feeding, selection of food types and textures, inappropriate mealtime behaviors, failure to adapt to age-appropriate food textures, and failure to only To name a few, self-sufficiency. Successful treatment of these feeding problems has many important implications for children with feeding problems, their families and society. Long-term chronic feeding problems and (a) child healthRisks are related to (b) increased perceived stress of children and families, (c) family mental health problems, (d) increased risk of eating for diseases such as anorexia, and (e) increased health care costs for children and families. Therefore, treating child feeding problems can lead to (a) improving the health of children, (b) improving the quality of life of children and families, (c) reducing mental health problems in the family, (d) reducing long-term risks-term diet problems, and ( e) Reduce medical care costs. Obviously, the nutritional needs of children who rely on technologies such as gastrostomy tube (G tube) have high medical care costs. For example, the health care costs of children who use the G tube in the first year are approximately US$41,811. Over the past two years, the child’s medical care costs are estimated to be US$78,811, and after five years, the cost will be US$189,811. These estimates are for simple care (for example, no other major medical issues related to gastrostomy) and do not include expenses related to home or individual treatment, which may be due to records in the families of children with feeding problems Caused by increased stress or psychopathology. In addition, if the child continues to need a gastrostomy tube for nutrition, or if the child has eating problems such as anorexia, the health care costs for these children may continue for many years. Williams and colleagues found that intensive behavioral therapy is a cost-effective alternative to long-term supplementary feeding. If the child continues to need a gastrostomy tube for nutrition, or if the child has eating problems such as anorexia in the future, the health care costs for these children may continue for many years. Williams and colleagues found that intensive behavioral therapy is a cost-effective alternative to long-term supplementary feeding. If the child continues to need a gastrostomy tube for nutrition, or if the child has eating problems such as anorexia in the future, the health care costs for these children may continue for many years. Williams and colleagues found that intensive behavioral therapy is a cost-effective alternative to long-term supplementary feeding. Intensive interdisciplinary treatment for feeding problems can eliminate the need for gastrostomy tubes and lead to age-typical feeding, which may end the need for continuous medical care in about 2 years. The estimated cost of intensive treatment of feeding problems is approximately US$5,420 in 2 years. Therefore, compared with the use of a gastrostomy tube to treat the problem, treating the feeding problem resulted in a savings of US$23,191 during 2 years, and a cost savings of at least US$134,191 compared to 5 years.
Therefore, not only can the quality of life be significantly improved for children with feeding problems and their families, but also when an interdisciplinary approach is used to treat feeding problems with behavioral analysis as the focus, it can also save a lot of costs.