Introduction
Fetal alcohol syndrome is a permanent birth defect syndrome caused by drinking alcohol during pregnancy. The disease is characterized by stunted growth, facial abnormalities, and unique clusters of central nervous system. The prevalence of FAS is estimated to be 1-3/1,000 live births in the general population and as high as 10-15/1,000 in high-risk groups such as foster care. Not all people exposed to alcohol and suffering from alcohol-related damage have FAS. Most people exhibit neuropsychological disorders without physical findings. It is now considered to be a multi-disease, FASD. FASD, partial FAS, alcohol-related neurodevelopmental disorders (Arnd) , static encephalopathy/alcohol exposure (SE/AE) and neurobehavioral disorders/alcohol exposure (ND/AE) all belong to the diagnosis of FASD.
Disciplines
Although claims about the harmful effects of maternal alcohol on infant outcomes date back to biblical times, the term Fas was not coined until 1973, and diagnostic guidelines were developed and refined in the 1970s and 1980s, that culminated in 1996 with the publication of the IOM guidelines. While the IOM guidelines reflect important progress, however, the IOM committee continued to feel that 1)“The medical diagnosis of FAS remains within the purview of the seismologist and clinical geneticist,”and 2) the guidelines are still deliberately broad and conceptual (gestalt) rather than specific and operational (as the case may be) . For example, central nervous system guidelines do not address how many defect areas must exist or the severity of the defect. The guidelines for facial phenotypes do not address how many features must exist, how severe each feature must be, or what measures should be used to determine its severity. Furthermore, the term ARND was coined in opposition to the withdrawal of the previous year’s Fae. Overall, the 1996 guidelines were not specific enough to ensure the accuracy of the diagnosis (the ability to arrive at a correct diagnosis) or the reproducibility of the diagnosis (the ability of two different clinicians to arrive at the same diagnosis for a given patient) .
Questions
In the absence of an accurate/reproducible diagnostic method, the diagnosis continues to vary widely between clinics. From a clinical perspective, diagnostic misclassification can lead to inappropriate patient care, an increased risk of secondary disability and missed opportunities for prevention. From a public health perspective, diagnostic misclassifications can lead to incorrect prevalence estimates. Inaccurate estimates impede efforts to allocate adequate social/educational/medical services to this high-risk population group, thus hampering an accurate assessment of prevention efforts. From a research point of view, diagnostic misclassification would prevent the examination of clinically meaningful comparisons between groups and the effective comparison of results between studies.
Research background
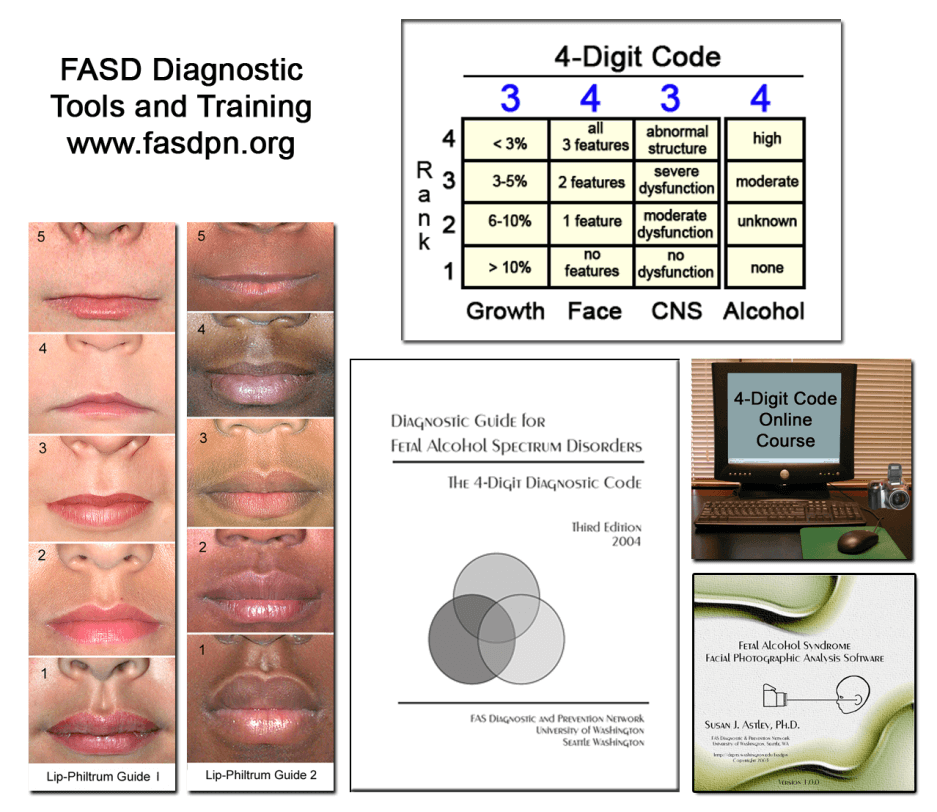
To overcome the limitations of the doctor-centred gestalt approach to FASD diagnosis, the FASDPN introduced an interdisciplinary team approach (doctors, psychologists, speech pathologists and occupational therapists) in 1993, the FASD 4-digit digital diagnostic code (FASD 4-DIGIT code) came into effect in 1997. In short, the four-digit number of the four-digit code reflects the extent of expression of the four key diagnostic features of FASD in the following order: 1) undergrowth, 2) Fas facial phenotype, 3) CNS structural/functional abnormalities, and 4) prenatal alcohol exposure (figure 1) . The order of expression of each feature is based on 4 points, of which 1 indicates that the feature does not exist at all, and 4 indicates that the feature exists seriously. Each level is defined on a case-by-case basis. Four-digit code ranges from 1111 to 4444. To date, each code combination has been observed in the FASDPN clinic, reflecting real differences in outcomes associated with prenatal alcohol consumption. A subset of 4-Digit Codes belonging to the FASD can be divided into three sub-groups with clinical significance and unique diagnoses:
FAS/Pfas (severe neuropsychological disorder with FAS facial phenotype) ;
SE/AE (severe neuropsychological disorder without facial phenotype) ;
ND/AE (no facial phenotype of moderate neuropsychological disorders).
Key research questions
The development of diagnostic guidelines requires validation of their performance before and after release. Performance should be validated by open empirical research. Performance metrics include accuracy, repeatability, effectiveness, and usefulness. Diagnostic teams should look for the following benchmarks in the current FASD diagnostic guidelines:
Are the guidelines evidence-based and drawn from a broad cross-section of the population? The evidence base should include performance validation prior to the release of the guideline.
Do the guidelines support an interdisciplinary approach to diagnosis?
Do the diagnostic criteria clearly and comprehensively define the case?
Can the diagnostic tool maximize measurement accuracy and accuracy?
Features of FASD (growth, face, central nervous system, alcohol) are not simply present or absent. Each exists along a separate, clinically meaningful continuum. Is this continuity reflected in the measurement and classification scale of the guide?
The validity of FAS diagnosis depends entirely on its unique facial phenotype. Therefore, the sensitivity and specificity of the FAS facial phenotype must be high (> 90%) and empirically confirmed. Do the facial standards in the guide meet these standards?
Do the guidelines identify the following diagnostic subgroups: A) clinically and statistically distinct from each other, b) reflecting an increased continuity of neuropsychological and physical abnormalities, and c) spanning the entire FASD continuum?
Is the diagnostic term to determine clinical integrity?
The validity of the scale for measuring and categorizing exposures and outcomes is demonstrated by its ability to detect statistically significant, physiologically meaningful correlations between physical, functional, and alcohol exposure levels. With the scales: does the face predict the brain? Is neurologic function related to neural architecture? Does the diagnostic subgroup have a distinctive alcohol-exposing style?
Are the guidelines readily applicable to clinical practice? Their usefulness should not come at the expense of their accuracy and precision. Training should be stopgap, affordable, universally available and competency-based.
Latest Research
Here is an example of how the FASD 4-BIT code meets all 10 benchmarks.
Evidence-based: the medical records of 1,014 patients (newborns, all races) in the statewide FASDPN who were evaluated for the diagnosis of FASD were used to develop a four-digit code. Its performance has been validated through empirical analysis and two years of use by interdisciplinary teams.
Interdisciplinary Approach: guidelines often require measurement and differential interpretation of physical (growth and deformity) and functional (mental, verbal, motor) outcomes in complex social/environmental settings. This requires the expertise of an interdisciplinary team.
Case definitions, measurement tools: exposure and continuity of results: case definitions, measurement tools: all conditions are specific/operational case definitions. For example, contrary to the IOM’s definition of the FAS facial phenotype (“Shape of features includes features such as short palpebral fissure (PFL) , flat upper lip, flat flat flat bone, and flat middle face”) , a 4-digit code defines how short, thin, and smooth the first three features must be, and provides tools (labp bone guide and FAS facial image analysis software) to accurately measure the integrity of these features. The 4-bit code also identifies whether the FAS facial phenotype exists or does not exist. The intensity of its expression is measured in four points.
Continuous exposure and outcomes: all FASD functions are measured and classified on a continuous or ordered scale. Lips and hair are measured at 5 Likert scale. The growth, face, central nervous system and alcohol levels were rated at 4 levels (Figure 1) . Even the diagnostic subgroups (ND/AE, SE/AE, and FAS/Pfas) reflect three distinct groups with increasing physical/functional impairment.
FAS facial specificity: the fourth-ranked FAS facial phenotype was more than 95% sensitive to FAS and prenatal alcohol exposure.
Unique diagnostic subgroup: MRI/MRS/fMRI has confirmed that ND/AE, SE/AE and FAS/PFAS are three clinically distinct and increasingly severe subgroups with distinctive alcohol exposure. For example, although both FAS/Pfas and SE/AE have severe dysfunction and disproportionately small caudates, only FAS/Pfas have a complete FAS facial phenotype and a disproportionately small frontal lobe, significantly lower neurocholine levels and significantly higher frequency and duration of alcohol exposure. Although SE/AE and ND/AE do not have complete FAS facial phenotype, SE/AE dysfunction is more serious, the proportion of caudate nucleus is disproportionate, and alcohol exposure is significantly higher. Although ND/AE has a moderate degree of dysfunction, MRI demonstrates a high prevalence of potential neurostructural abnormalities.
Terminological integrity: the terms SE/AE and ND/AE replace the terms ARND and Fae in order to accurately record an individual’s results and exposures without implying that a causal relationship has been established (or excluded) between the two.
Effectiveness: published empirical studies document a broad, physiologically sound relationship between exposure and outcome. Some examples: Face Prediction Brain: IQ and regional brain volume decreased significantly with increased expression of the FAS facial phenotype (grade 1-4) . Neural function correlates with neural structure: the 3 point scale of central nervous system dysfunction (grade 1 = none, grade 2 = moderate, grade 3 = severe) correlates closely with a reduction in the caudate nucleus.
Easy to practice: guidelines and tools can be distributed online free of charge or at cost. Training is online, certified, low-cost, and can be done over the weekend.
Research Gap
The initial obstacles to FASD diagnosis (outlined above) have now been overcome through rigorous diagnostic guidelines implemented by interdisciplinary teams. It is time to focus on the FASD intervention.
Conclusion
The FASD 4-DIGIT Digital Diagnostic Code provides an intuitive logical digital approach to reporting results and exposures, reflecting the true diversity and continuity of disability associated with prenatal alcohol exposure. By using quantitative scales, specific case definitions, and an interdisciplinary team approach, it also provides greater accuracy, accuracy, and effectiveness than the Gestalt approach.
Impact on parents, services and policies
Parents (13 years and older than 830 years) were highly satisfied with the FASDPN interdisciplinary diagnostic method using a 4-digit code. They reported that the method was easy to understand and provided them with information that was not available elsewhere (99% recommended the clinic to others) . FASDPN strategic type has also won the respect of service providers throughout the state. The diagnostic report provides detailed information and directions for providers to qualify children for services. Parents of children with FAS/Pfas, SE/AE and ND/AE are recognized to benefit from recommended interventions. Interdisciplinary and four-digit codes of law have been adopted worldwide, often initiated and supported by legislative policy.